Vaccination in Singapore runs on a simple thesis: prevention succeeds when policy, logistics, and affordability align. The NCIS and NAIS are the policy spine, translating evidence into age-based and risk-based recommendations. Clinicians then personalise the timing for pregnancy, chronic conditions, or occupational exposure.
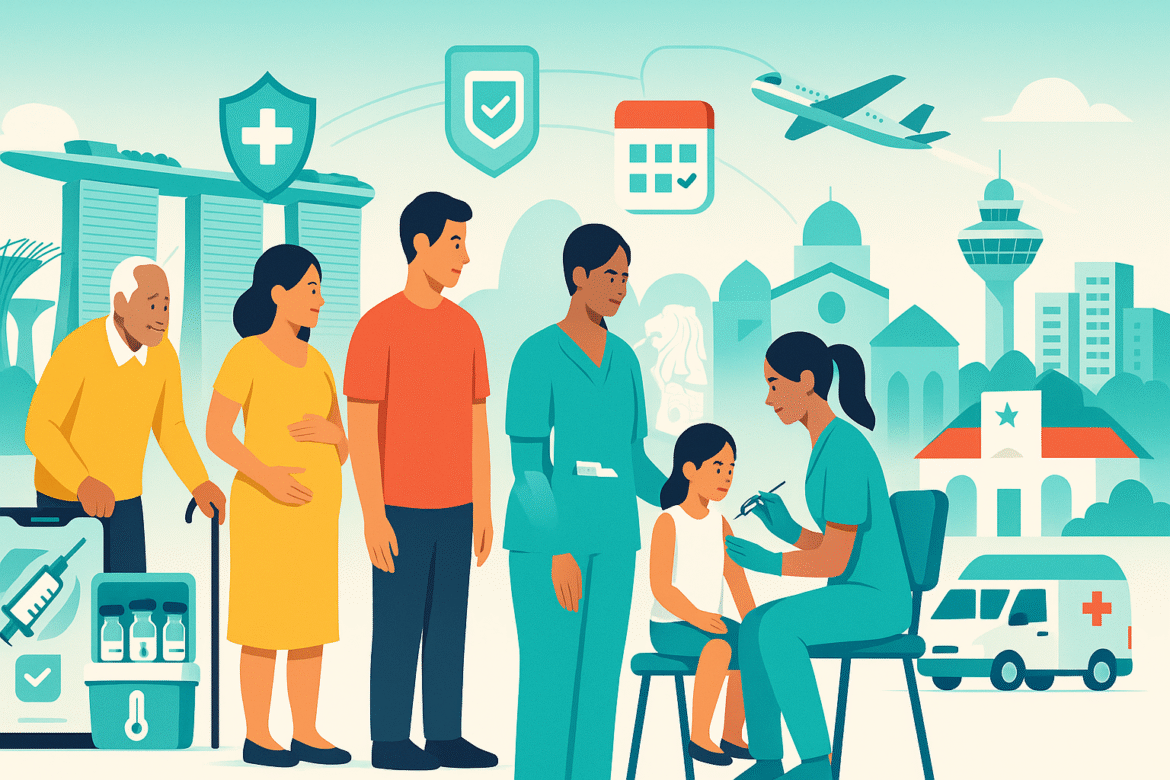
Equity is engineered into delivery. Polyclinics offer subsidised access; CHAS-participating GPs bring services closer to homes; school-based teams ensure adolescents don’t miss HPV. Mobile outreach and extended hours reduce time costs for shift workers and caregivers. When convenience improves, coverage follows.
Financing keeps the door open. Targeted subsidies apply at public providers, and approved adult vaccines under NAIS can be paid with MediSave withdrawals, lowering immediate expenses for seniors and those managing chronic illness. Price transparency, published fee schedules, and clear counseling prevent unpleasant surprises at the counter.
Data drives targeting. The National Immunisation Registry benchmarks cohorts and flags gaps for catch-up. During campaign pushes, analytics highlight neighborhoods with lower uptake so planners can deploy mobile teams or collaborate with community groups. HealthHub reminders and SMS nudges convert good intentions into kept appointments.
Safety governance sustains trust. Providers follow screening checklists, discuss common and rare side effects, and report adverse events to HSA’s pharmacovigilance system. Cold-chain integrity is audited: vaccine fridges are tagged, temperatures are logged, and staff are trained in contingency steps if excursions occur. This diligence is invisible when everything works, yet it’s central to public confidence.
COVID-19 stress-tested the apparatus. Singapore scaled venues, mobilised volunteers, and communicated in multiple languages, knitting public and private capacity. Those lessons now inform seasonal influenza campaigns and adult pneumococcal drives, especially for older adults and people with diabetes, lung disease, or heart conditions.
Engagement is multilingual and respectful. Outreach materials arrive in English and vernacular languages; frontline staff answer questions without dismissiveness. Myths are addressed with data and empathy, recognising that trust is earned in conversation, not demands.
The payoff is broad immunity and fewer vaccine-preventable outbreaks. Children enter school protected against measles, mumps, rubella, diphtheria, pertussis, polio, Hib, and pneumococcal disease. Adults are increasingly protected against influenza, pneumococcal infections, and HPV-related conditions. The system’s real achievement is reliability: people know what to do and where to go, year after year.