Singapore’s approach to healthcare technology is less about flashy gadgets and more about stitching together the care continuum. The National Electronic Health Record anchors this strategy, offering clinicians a longitudinal view across polyclinics, GPs, hospitals, and ancillary providers. When a senior with diabetes presents with breathlessness, the care team sees glucose trends, renal function, and a history of heart failure—all before ordering tests—improving decisions and reducing delays.
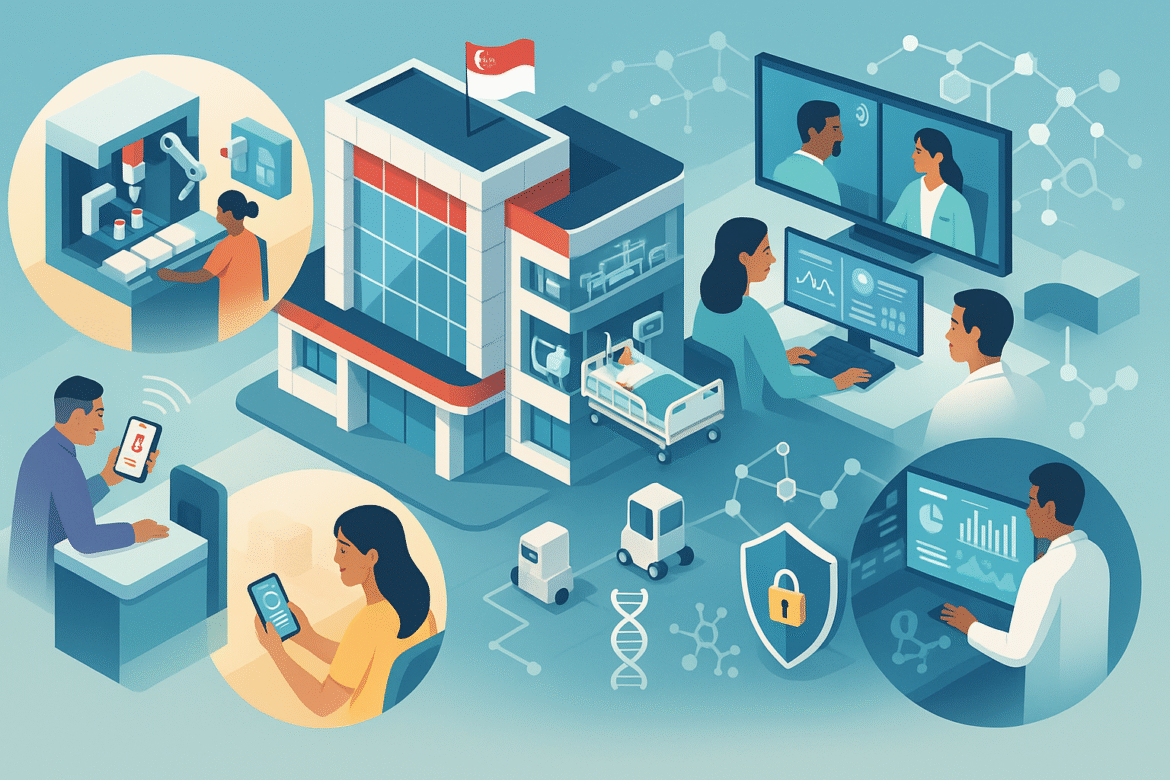
Public-facing tools complement the clinical stack. HealthHub functions as a personal health organiser: people check lab results, track vaccinations, and settle bills without standing in lines. Appointment reminders and digital consent reduce missed visits, which is essential for chronic disease management. Telemedicine platforms slot into this flow, supporting follow-ups, medication reviews, and allied health services like physiotherapy and dietetics. Virtual care reduces travel friction and supports caregivers who cannot leave work or home easily.
Diagnostics are a major beneficiary of AI. Algorithms triage images for urgency, screen scans for subtle findings, and pre-populate structured reports. In pathology, digital slides enable remote consults and quality audits. However, Singapore’s regulatory posture emphasises clinician oversight, local validation, and post-market surveillance. The message is clear: augmentation, not replacement.
Inside hospitals, automation boosts reliability. Pharmacy robots manage dispensing for high-volume medications; barcode systems ensure correct matching of patient, drug, and dose; and smart infusion pumps cross-check orders against electronic protocols. Logistics robots move supplies, while predictive maintenance keeps critical equipment from failing at the bedside. Wards deploy continuous monitoring patches that feed early warning algorithms, enabling nurses to intervene before deterioration escalates to a code.
On the data side, interoperability is an ongoing programme rather than a one-off project. Vendors are nudged toward open standards; APIs allow third-party innovators to integrate securely; and data governance frameworks define what’s shared, with whom, and for what purpose. Cybersecurity is tightly integrated—identity and access management, encryption, and incident response exercises reflect the sector’s criticality.
Primary care sits at the center of population health initiatives. Remote monitoring devices flow data back to clinics, where team-based care reduces hospitalisations. Pharmacogenomic screening is being introduced in targeted contexts, ensuring safer prescribing for specific patient groups. Meanwhile, analytics identify high-risk cohorts for proactive outreach—patients recently discharged, or those with deteriorating control of chronic conditions.
Human factors round out the picture. Clinicians help design interfaces; alerts are tuned to reduce noise; and change management plans anticipate the learning curve. Patients receive help through community health workers and walk-in counters for digital onboarding. Inclusion matters: multilingual options and caregiver proxies keep older adults engaged in their care.
Singapore’s synthesis of records, robotics, remote care, and regulation delivers cumulative gains: fewer handoff errors, faster diagnostics, smoother discharges, and more care occurring safely at home. The technology impresses less by spectacle and more by how well it disappears into daily practice.